Delegation
Delegation involves authorizing team members to perform controlled acts outside of their typical scope of practice. Team members you are delegating to must have the appropriate training to perform the act safely.
Delegation and supporting team-based care
Delegation of controlled acts can support a team-based approach to the delivery of care.
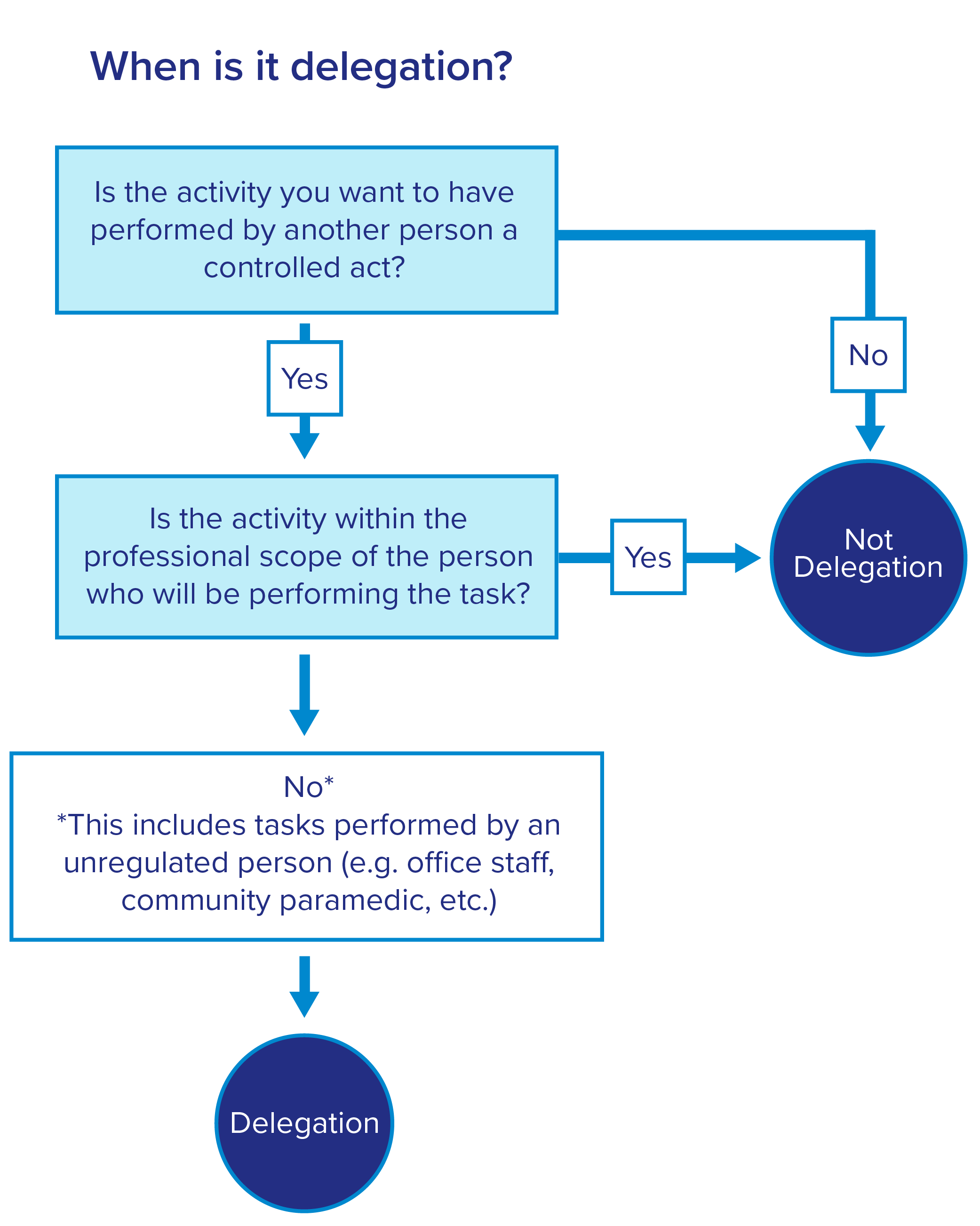
See a flow chart to help you determine if an activity is delegation.
Appropriately delegating controlled acts to health-care team members, both within your own organization and across organizations (e.g. family health team, community health centre, home and community care), can support patients in accessing the care they need when they need it.
Delegating controlled acts can increase your ability to work at your optimal scope, while providing support and supervision to other team members who have the knowledge and skills to perform delegated controlled acts with competence and appropriate care.
On this page
Controlled acts
When is it delegation?
How to delegate
Risks involved in delegating
Billing for delegated services guide
Controlled acts
There are 14 controlled acts under the Regulated Health Professions Act (RHPA). These are acts that can only be performed by regulated health professionals whose scope includes authorization to perform the act. For example, pharmacists are authorized to dispense a drug; and midwives are authorized to deliver a baby.
If a physician wants another person to perform a controlled act, delegation will be required when:
- The act is not within the scope of the regulated health professional who will be performing the act, OR
- The person performing the act is an unregulated person
When is it delegation?
Not all activities that you direct other staff to perform are considered delegation.
It is only delegation if the activity being assigned is:
- A controlled act, and
- Not within the scope of the regulated health professional who will be performing the activity, or the person performing the activity is an unregulated person
Being able to delegate a task does not automatically mean you can bill for it. Refer to the OHIP Payments for Delegated Procedures quick reference guide for details.
Use this flow chart to help you determine if an activity you are directing other staff to perform is delegation.
Delegation
![]()
The activity being assigned is a controlled act, and
The activity being assigned is not within the scope of the regulated health professional who will be performing the activity, or the person performing the activity is an unregulated person
For example, your patient, Jane, is coming for allergy testing. Instead of testing her yourself, your nurse, who is trained in the procedure, conducts the testing.
This is an example of delegation because allergy testing is a controlled act that is outside the nurse’s typical scope of practice.
Not delegation
![]()
The activity being assigned is not a controlled act, or
The activity is a controlled act, and it is within the scope of the regulated health professional who will be performing the activity
For example, your patient, John, is coming for a COVID-19 vaccine. Instead of vaccinating him yourself, your nurse practitioner gives him the vaccine.
This example is not delegation because vaccination is within the nurse practitioner’s typical scope of practice.
Become familiar with the scope of your team members
Learning about the scope of your team members will tell you which controlled acts they can perform without delegation. If a particular controlled act is not in their scope, delegation is required for them to be able to perform it.
Examples of regulated interprofessional team members’ scope include:
- Registered practical nurses, nurses and nurse practitioners: Scope of practice (CNO)
- Pharmacists: Legal authority for scope of practice/authorized acts (OCP)
- Physiotherapists: Physiotherapy act (see section 4, authorized acts) (Government of Ontario)
- Social workers: The only controlled act that social workers are authorized to perform without delegation is the controlled act of psychotherapy (number 14)
- Physician assistants: As of April 1, 2025, only individuals registered with the CPSO may use the protected title of ‘physician assistant’. Although physician assistants are now regulated, their scope of practice has not changed. Delegation is still required for them to perform any controlled acts
- Medical laboratory technicians: The only controlled act that medical laboratory technicians are authorized to perform without delegation is taking blood samples from veins or by skin pricking
- Audiologists: The scope of practice of audiologists includes selecting, prescribing, fitting and evaluating amplification devices, including hearing aids and surgically implanted devices such as cochlear implants and bone-anchored hearing aids. Since it is within their scope of practice, audiologists can prescribe hearing aids without delegation – no physician sign-off on hearing aid funding applications is required. However, Hearing Instrument Practitioners (HIPs) are unregulated health-care professionals, and therefore cannot prescribe hearing aids
How to delegate controlled acts
Direct orders and medical directives are two ways to delegate controlled acts. Typically, delegation takes place through medical directives; however, there will likely also be situations in your practice that are not covered by a medical directive where a direct order will be needed.
Risks of delegation
The risks of delegating and performing controlled acts vary depending on the act being performed and the circumstances. Physicians are responsible for knowing these risks before delegating. Physicians must evaluate the circumstances and the choice to delegate to ensure patient care is provided safely and effectively in accordance with CPSO policy expectations.
Physicians should contact the CMPA if they have questions about liability protection related to delegation. As an employer, a physician may also be liable for the actions of their employees with respect to medical negligence. In some circumstances, employees may carry their own insurance for the services they are providing.
To protect yourself, document every step of the delegation process, including any care provided to patients through an order or medical directive.
- Read more about when can you safely delegate from the CMPA.
Contact the CMPA if you want more information on protection available when delegating through direct orders or medical directives.