Prescription for Ontario: Doctors’ Solutions for Immediate Action
The OMA has released 11 pragmatic solutions to address the top three issues facing the health-care system, following extensive consultation with physicians, stakeholders and the public. This Solutions Report is the latest in our Prescription for Ontario advocacy series. Our original document had 87 recommendations. In spring 2023, we released our Progress Report and were pleased to share that action had been taken on 51 of our 87 recommendations, but there is still much left to do.
The top three urgent priorities that have since risen to the top are:
- Fixing the crisis in primary care to ensure everyone has access to a family doctor
- Addressing the growing burden of unnecessary administration
- Increasing community capacity and tackling hospital overcrowding
Far too many Ontarians, a staggering 2.2 million people, are without a family doctor. That is roughly the combined populations of London, Thunder Bay, Ottawa, Hamilton and Kingston without access to comprehensive preventive care.
Physician burnout is a critical issue facing the health-care system and it is increasing at an alarming pace. Too much time is spent on paperwork, not patients.
At the same time, too many acute-care hospital beds are occupied by patients whose acute medical issues are stable and can be discharged but lack the appropriate support in the community.
Read this page for more information on our solutions, which will guide our advocacy efforts in the coming weeks and months. While they will not solve every issue, taking Ontario doctors’ advice today will get the system out of crisis mode tomorrow. Then, we can shift our focus back to implementing the other transformative recommendations outlined in our original Prescription for Ontario.
Learn more about the work of Ontario's Doctors
Stay informed on how Ontario’s Doctors are working to improve health care and how you can support.
Tracking government action
The OMA produced a progress report on the implementation of the original Prescription for Ontario. See how doctors' expertise is making an impact.
Fix the crisis in primary care
The number of Ontarians without a family doctor is growing steadily and this situation has long surpassed crisis levels. Right now, one in five Ontarians are on track to be without a family doctor in the next two years.
A study conducted by INSPIRE-PHC shows that as of March 2022, 2.2 million Ontarians were without a family doctor, up from 1.8 million in March 2020.
Further exacerbating the problem, 40 per cent of family physicians say they are considering retiring in the next five years, according to the 2022-23 OMA member survey. A new survey by the Ontario College of Family Physicians found that two-thirds of its members plan to change their practice model, reduce their hours or retire in the next five years.
The solutions
Patients with complex health needs often must see many different health-care providers in addition to their doctor. Very few have access to team-based primary care, which consists of inter-professional health-care providers, each working to their full scope of practice to provide comprehensive primary care services to patients in their community. Even for those with access to other providers, this care is not always well co-ordinated and holistic for patients. It can be disjointed and fragmented, which leads to inefficiencies in accessing care and increased cost. Unfortunately, most Ontarians don’t have access to these other providers altogether. Every Ontarian, no matter where they live, should have a well co-ordinated health-care team supporting them when and where they need it.
“Done right, interprofessional primary care teams can increase clinician capacity to serve more patients, improve joy in work for clinicians and improve quality of care for patients” — Dr. Tara Kiran, family doctor, Toronto

While the Ontario government’s investment of $30 million to expand access to team-based care is a welcome start, this amount is not commensurate with the team-based-care needs in the province. Only 30 per cent of Ontario’s family doctors practise in models with access to government-funded team-based support, meaning the vast majority do not have the team support they need. To improve primary care delivery, we ask the province to:
- Build on its investment and further expand team-based care across the province
- Equip the remaining 70 per cent of family doctors who do not have access to primary care teams with equal access to a team of providers for their patients by building on its $30-million investment to expand and create new interprofessional teams
To ensure successful creation and implementation, the OMA envisions that these teams should:
- Be tailored to meet the needs of the patients in the community being served (at minimum, the team should include a physician, nurse, administrator and at least two other inter-professional care providers, such as a social worker, registered dietitian, nurse practitioner, physiotherapist, pharmacist, specialists and mental health professional and/or outreach worker)
- Have cross-coverage and access to locum support – the equivalent of a substitute teacher in the school system – so patients still have access to physician care when their doctor is away
- Be linked digitally and seamlessly to facilitate care co-ordination and increase the time that family physicians spend on direct patient care, meaning that teams do not need to work out of the same location
- Be funded by the government and adjusted based on the specific, unique care needs of a community, rather than a one-size-fits-all approach
- Have family physicians play a key role in the leadership structure and be provided with additional training and funding for performing these duties rather than doing so off the side of their desk
- Prioritize access for equity-deserving patients who need comprehensive team-based care the most
Benefits for patients
Patients not requiring physician care could see the most appropriate and skilled provider for the care they need. For example, a patient can see a dietitian rather than a physician for nutritional and diet advice. This support could improve continuity of care and allow family physicians to take on more complex unattached patients, see them faster and free up more time to provide medical care.
Cross-coverage allows patients to receive continued access to care when a provider on the team is away, instead of having to go to a walk-in clinic or emergency department. Evidence also suggests that this type of comprehensive care can improve health outcomes, patient satisfaction and offer more patient-centred care.
Benefits for physicians and the system
Physicians often feel a moral obligation to be an expert in areas in which they are not trained when they don't have access to a team to which they can refer patients. Knowing other team members are caring for the patient allows doctors to be doctors. This would also free up time, helping to alleviate burnout.
Primary care teams lead to reduced system costs by diverting patients from costly emergency department visits, reducing time spent in hospitals, identifying issues earlier and promoting healthy living. Evidence from British Columbia suggests that a very sick patient without access to high quality primary care can cost that province’s system $30,000 per year. When attached to a comprehensive family care model, the same patient can cost just $12,000. Extrapolating to Ontario, where there are currently so many patients without team-based care, there would be significant cost savings to the overall health system if team-based care became the norm.
The primary care team model also improves care co-ordination by increasing communication between health-care providers through a shared electronic medical record. Such system integration is lacking in other care models in Ontario. Seamless information-sharing improves communication among care providers, reduces conflicting advice and facilitates data transfer between providers.
Ontario’s rural and northern communities face profound physician shortages due to chronic recruitment and retention challenges.
According to the Northern Ontario School of Medicine University, communities in northern Ontario are actively recruiting more than 350 physicians, including more than 200 family doctors. This does not reflect actual health-care needs, which are increasing. With half of the physicians working in northern Ontario expected to retire in the next five years, according to NOSM, this situation will only worsen. Many are also considering adjusting their clinical practices, due to the lack of work-life balance, resources and supports.
Many northern and rural emergency departments are at risk of closure as a result. Family doctors, who also provide emergency care in the north, have unsustainably high workloads and are forced to sacrifice their primary care practice to keep emergency department doors open. This has dire consequences for patient outcomes and puts physicians at increased risk of burnout. To make a lasting impact on physician shortages and understaffed emergency departments, we ask the province to build a comprehensive physician workforce strategy with four key action areas: retain, recruit, return and plan for the future.
Retain
It is daunting to be the only physician in a community without appropriate peer support and networks, such as those that exist in urban settings. While virtual and remote care options have improved some circumstances, more needs to be done to implement support networks, hubs of care providers and other innovative solutions to enable physicians to practise confidently in rural, remote and isolated communities. The OMA emphasizes the importance of reliable, accessible supports, such as a sufficient pool of qualified locums available when physicians need to be away from their practices (for example, for illness, continuing education or vacation). We advocate for the creation of a provincial locum pool. The OMA also agrees with the Ontario College of Family Physicians that locum recruitment needs to be scaled up and supported via coaching, a streamlined credentialling process and appropriate travel expense coverage.
Recruit
The OMA welcomed the Ontario government’s announcement of the Practice Ready Ontario assessment program, which aims to add at least 50 new internationally educated family physicians into the system by 2024. To meet the growing need for family physicians, we call on the province to build on its momentum and license more internationally educated physicians.
Return
Some physicians have moved away from the practice of comprehensive office-based family medicine, away from practice in rural and remote regions and toward more narrowed scopes of practice. Encouraging physicians to return to the areas and types of practice most required by Ontario communities will help to build a more stable and sustainable health system, and it should be a top priority.
“Rural general practice is uniquely difficult for several reasons. It requires a broad scope of knowledge and skills, courage to face whatever rolls through your doors and an ability to improvise with what you have — all while being isolated from physician colleagues. There is a limited number of physicians who want to practise rural medicine and even fewer who are willing to come to rural communities. To ensure that these physicians stay practising in rural communities, they need to be adequately supported in the office, emergency department and hospital, and remunerated appropriately for the difficult work they do” — Dr. Dannica Switzer, northern rural locum, Wawa, Ont.
Plan for the future
Ontario needs a data-driven health workforce planning framework to understand the current and future physician workforce requirements in the health-care system, determine the supply, mix and distribution to meet these needs and identify the policy levers and investments required to build a sustainable system. The OMA is developing a groundbreaking tool using artificial intelligence called PRIME (Physician Resources Integrated Model) that projects future health-system needs and capacity, such as how many family physicians and specialists will be required to meet patient needs in a specific geographic area. We ask the Ontario government to work with us on using PRIME to help address current and anticipated health human resources challenges, so that Ontario is better prepared to respond to emerging HHR challenges and avoid future crisis situations.
Benefits for patients
A physician workforce strategy could help improve access to care in northern and rural Ontario, enabling people to receive high-quality primary or emergency care closer to home. Patients in the north face persistent inequities in the care they receive and in their health outcomes, compared to people living in other regions of the province. Focused action from policymakers to resolve the physician shortages could help bring stability and begin to address the health gaps in the north, and increase access to family doctors for Ontario patients.
Benefits for physicians and the system
Health workforce planning benefits physicians by identifying resource and capacity challenges and examining scenarios or measures to address them. Improving health workforce and system capacity will alleviate the burden on beleaguered physicians, improve work-life balance and future-proof the workforce.
A data-driven, evidence-based workforce strategy will improve system efficiency and help Ontario meet the current and future population's health-care needs. Regular monitoring and evaluation will help to address emerging challenges, match physician supply and skills to population needs and improve system sustainability into the future.

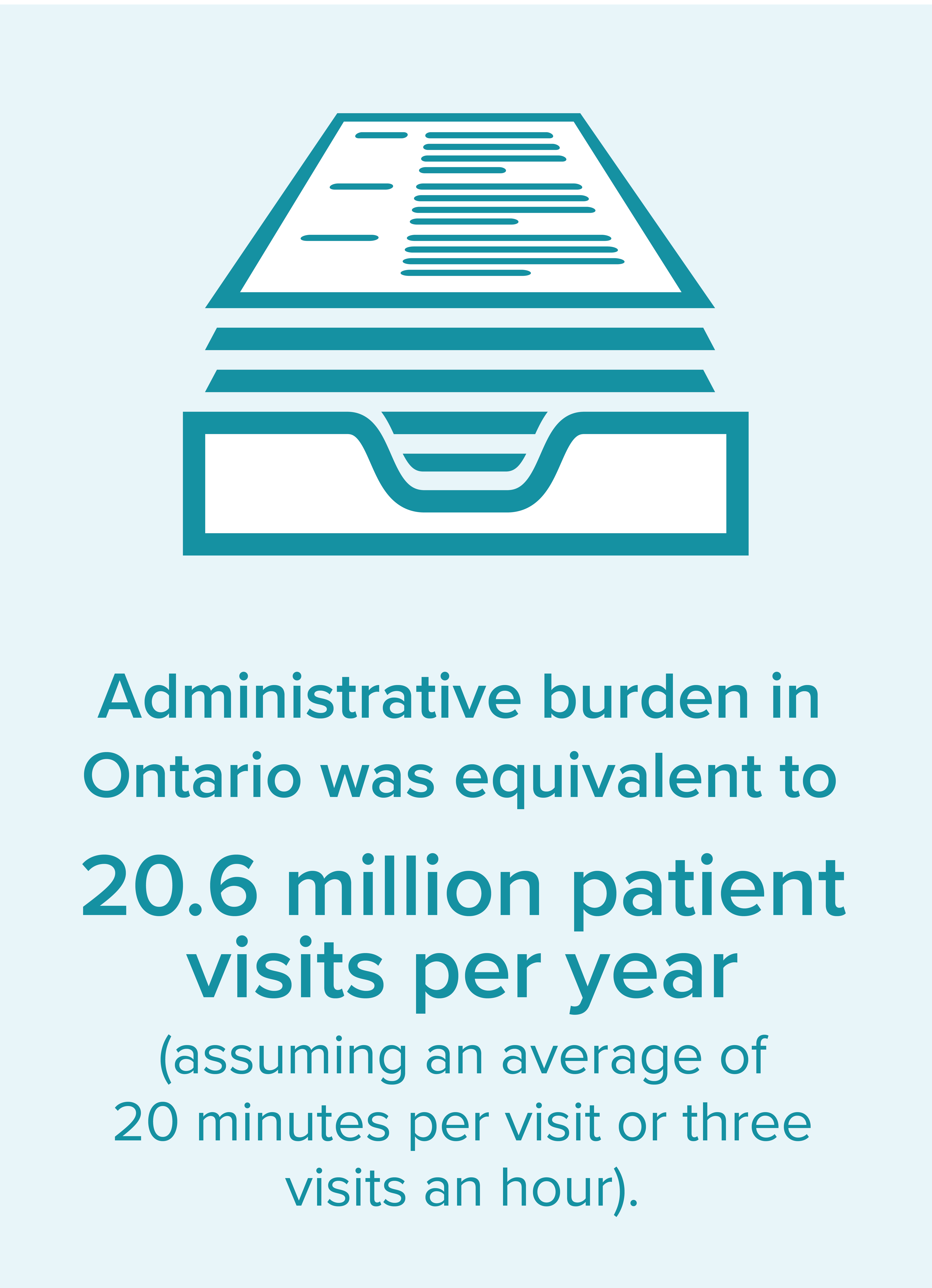
Reduce the burden of unnecessary administration
Physician burnout is a critical issue facing the health-care system and it is increasing at an alarming pace. Immediate action is required to reduce administrative burden and let doctors be doctors.
Among physicians surveyed by the OMA, almost three-quarters (72.9 per cent) said they experienced some level of burnout in 2021, up from 66 per cent the previous year. Just over one-third (34.6 per cent) reported either persistent symptoms of burnout or feeling completely burned out in 2021, up from 29 per cent in 2020.
Our 2022-23 member survey revealed that 40 per cent of physicians are considering retiring in the next five years. Simply put, we must do everything we can to retain those physicians who are considering retiring early due to burnout.
The solutions
Most family doctors cannot easily refer their patients to the appropriate specialist with the shortest wait time in their area, which can mean longer wait times for patients. To ensure equitable and timely access, a centralized intake and referral system should be managed by Ontario Health and implemented in collaboration with the OMA, Ontario Health Teams, hospitals, community-based surgery and diagnostic clinics, and primary care practices. It must be created with strong physician involvement to help build a solution that works for patients and physicians. It must also preserve patient choice and maintain capacity for certain specialists who provide targeted care to equity-deserving populations.
Benefits for patients
Patients could choose the shortest wait time in their area or a preferred surgeon/specialist, based on known wait times. Patients would no longer be left waiting for weeks/months for their physicians to repeat the search-and-referral process multiple times until a successful referral is made.
“A centralized intake and referral system is the single most important step in eliminating long wait times for surgery in Ontario. Without a centralized model to balance clinical loads, no other measure — not even increasing surgical capacity by creating community-based surgical facilities — can prevent the longest waits that are happening in our system. Moving toward single-entry models and team-based care also improves the work-life experience for specialists, reduces professional inequities and gender-based referral biases, and improves the reliability and quality of patient care” — Dr. David R. Urbach, surgeon, Toronto.
Benefits for physicians and the system
Family physicians would no longer have to contact specialists in their area one by one to find someone who can treat their patient in an appropriate timeframe, while completing different specialists’ intake forms each time.
Such a system will also improve the experience for specialists who often report receiving referrals for care that they do not provide. In addition, while some specialists may have a large referral base, others may experience a bias in referrals. For example, an OMA study released in August 2023 found that male specialists receive more referrals than female specialists with all other factors controlled and that a centralized referral system could help to close this gap.
A centralized intake and referral system could also reduce provincial wait times by maximizing the efficiency and capacity of all specialists.
The unrelenting demands for physicians to complete forms, sick notes and referral letters continue to increase. This includes forms from multiple sources, such as different levels of government, various government ministries, employers and insurance companies. It also includes employers’ requirements for sick notes and physician referrals for patients to use their benefits for paramedical services such as physiotherapy and registered massage therapy.
Many forms have unnecessary or repetitive questions and challenging turnaround times. Some assessments or requests are not within physicians’ scope yet still require their time and sign-off. The problem is even more challenging because countless portals, each requiring a separate log-in, have been established to access some of these forms. They are not integrated with existing electronic medical records, which is yet another source of administrative burden for physicians.
Benefits for patients
Reducing administrative minutiae in a care interaction will improve the experience for patients. With more time, doctors may be able to see more patients. Ensuring that the right provider is filling out the correct form can also reduce errors on forms and cumbersome back-and-forth, and help patients get what they need more efficiently. Removing employer requirements for sick notes and paramedical referrals will open up appointments for patients requiring physician care, will enable patients to get paramedical care more easily and more quickly, and will help patients stay home when they are sick, thereby protecting their co-workers. This will also keep more infectious patients out of physicians’ waiting rooms when physician care isn’t required.
“Genuine progress on forms is being made, thanks to the leadership and advocacy of the OMA Forms Committee and collaborative commitment from the Ministry of Health. Now is the time to build on this momentum and address the administrative burden due to forms” — Dr. Scott Elliott, Brantford, and chair, OMA Forms Committee
Benefits for physicians and the system
Physicians would have more time to see patients, enhance their own wellness and work-life balance or a combination of both. They would also have greater professional satisfaction, allowing them to do what they went into medicine to do.
As addressing administrative burden was ranked by Ontario physicians as the highest-priority solution to burnout, the OMA implores the province to implement these recommendations to make significant improvements in physician burnout. This is essential for physicians’ well-being as well as for the sustainability of the Ontario health-care system, considering the province’s health human resources challenges.
Physicians spend a significant portion of their working hours on administrative tasks, including documentation, order entry, billing and coding, which detracts from their ability to provide direct patient care. We must find concrete solutions to address this issue and improve the well-being of our physicians.
That’s where AI scribes could make a difference.
A proposal submitted by OntarioMD and the eHealth Centre of Excellence presents a comprehensive approach to evaluate the implementation of AI scribes and automation processes, to alleviate the increasing levels of burnout experienced by primary care physicians in Ontario.
The potential impact of AI scribes is high, but their value is not yet fully understood, especially within the Ontario context. The project by OntarioMD and partners aims to identify, refine and validate these technologies’ potential impact on providers, patients and the Ontario health system. It will also develop a strategy to promote the greatest level of adoption in primary care to maximize the impact on system capacity.
We ask the province to fund this proposal. The proposed budget is $4.2 million over two years.
Benefits for patients
When a doctor spends less time documenting, that means more time for one-on-one engagement with patients, which could improve patients’ experiences engaging with doctors.
Benefits for physicians and the health-care system
Automated processes could significantly reduce time spent on after-hours documentation, freeing up time for more patients and/or enhancing work-life balance.
It is vitally important that appropriate clinical information be shared between hospitals and community-based family physicians to support the best clinical care for patients. Without access to this information, family doctors may not have the full picture of their patients’ health.
Health Report Manager (HRM®) is an important provincial digital asset that enables this communication and reduces fax use. To maintain its value, some HRM functions need improvement to better meet the workflow needs of primary care physicians.
The recommendations, recently released by the HRM Task Force, include:
- Establishing and implementing information standards for reports from sending facilities, such as hospitals
- Allowing primary care physicians more choice in the types of reports they receive
- Improving integration of HRM into existing clinical tools such as electronic medical records
Physicians consulted by the task force said these enhancements must be adopted quickly to maintain the high value of HRM and reduce the administrative burden of the tool.
“I love seeing my patients. Timely, efficient reports via HRM should support physicians spending time with patients rather than scrolling through long and duplicative reports. Patients are right to expect hospitals, specialists and diagnostic services to efficiently communicate important clinical information to their family physicians to inform ongoing care. The province must prioritize the recommended changes to HRM to establish information standards for reports, more choice in reports received, and better integration into existing clinical tools. Failing to do so would be a significant patient safety risk and would further exacerbate unnecessary administrative burden for family physicians” — Dr. Jocelyn Charles, family physician, Toronto, and member of the HRM Task Force Steering Committee
Ontario Health has started implementing these recommendations in partnership with OntarioMD, which is a strong first step.
We request that the province prioritizes this work and aligns resources through Ontario Health to quickly implement these recommendations to ensure that benefits are seen at the clinical level provincewide.
Benefits for patients
When patients move between care settings (for example, from the hospital back to their home), it is important that the appropriate clinical information be shared with their primary care doctor.
Benefits for physicians and the health-care system
A high-functioning HRM system ensures that primary care doctors receive the right information, in the right format, in a way that does not contribute to their administrative burden, enabling them to deliver the best quality care.

Increase community capacity and tackle hospital overcrowding
Far too many Ontarians are languishing in hospital beds when they could be discharged and better cared for elsewhere. One significant cause of hospital overcrowding is a lack of access to home care, long-term care and palliative care. For example, a patient with dementia requiring supportive care provided by a long-term care home ends up living in a hospital because there is no space for them where they need to be.
This bottleneck of patients, referred to as alternate-level-of-care, has existed in Ontario for many years, with its root causes remaining unresolved. The pandemic made a bad situation even worse and now the consequences of inaction are more urgent than ever.
The solutions
When physicians refer patients to home care, they are often accepted right away, yet they may need to wait several weeks or months to receive a small amount of care.
In an August 2023 poll of OMA members, respondents identified long wait times as the top barrier physicians face when trying to access home care for their patients. They also identified the lack of system navigation support, lack of access to appropriate levels of care and inadequate integration within the entire health-care system as top barriers.
There simply are not enough professionals, nurses and personal support workers who can provide this necessary care. Instead, we rely on informal caregivers – for example, partners, family members and friends – to provide this care.
“On behalf of the Ontario Community Support Association, we appreciate being consulted by the OMA on the importance of home and community care. Investing in this key sector will lead to better outcomes and reduced pressures on long-term care and our hospitals. It is also essential that home and community providers work more closely with primary care to ensure more integrated and co-ordinated patient care” — Deborah Simon, chief executive officer, Ontario Community Support Association
One of the root causes behind home-care staff shortages is the significant wage differential between home care and other sectors. The Ontario government must accelerate its efforts to recruit and retain home-care staff, which means paying them a wage that makes it abundantly clear just how vital they are.
Benefits for patients
Patients would receive timely and appropriate amounts of care that matches their needs.
Benefits for physicians and the system
With more appropriately funded home-care services and greater capacity, we will avoid patients ending up in hospitals. Physicians’ patients would receive home care in a timelier manner. We would also see greater staff retention in the home-care sector and hopefully less burnout.
“Hospital at home” programs provide therapies, tests and monitoring typically provided in hospitals for patients who are sick enough to require acute care, but stable enough to receive them at home. These programs involve home visits, remote monitoring and 24/7 access to health-care professionals. With this approach, care such as oxygen therapy, intravenous fluids, intravenous antibiotics and respiratory therapy can be delivered safely in the home. In Canada, only British Columbia and Alberta have formally implemented programs like this. In Ontario, this has only been implemented on a small scale in Hamilton and Erie St. Clair and this model should be expanded.
“Bringing more care into the home – from traditional home care to more intensive supports that can provide palliative, long-term care and even hospital-level care at home – is the only way Ontario can truly tackle its chronic hallway medicine and ALC issues. Bringing the right care to where people want to receive it – in their own homes – is not only more cost-effective, but also what the system and its users need” — Dr. Samir Sinha, geriatrician, Toronto
Benefits for patients
Patients can receive hospital-level care in the comfort of their own homes. These patients report high levels of satisfaction.
Benefits for physicians and the system
These programs reduce pressures on hospital services. In Victoria, Australia, the program added the equivalent capacity of a 500-bed hospital without building one and paying for capital costs. The Johns Hopkins Hospital at Home program found that the total cost of the program was 32 per cent less than traditional hospital care, and the mean length of stay was shorter by one-third. These programs also achieve higher levels of provider satisfaction.
Home care needs to be integrated within a team-based care model, which could be done by embedding both care co-ordinators and home-care professionals in Ontario Health Teams. Care co-ordinators could be integrated with primary care teams, and could support all members of the OHT, including hospitals, family health teams, solo-practice physicians, long-term care homes and others. Physicians could work with a dedicated care co-ordinator, whose caseload should be aligned with the physician-patient roster to support better communication in the health-care team. Anecdotally, the top complaint from physicians when talking about care co-ordination is the lack of effective and efficient communication among physicians, care co-ordinators and home-care providers.
Benefits for patients

Continuity of care could be better maintained if nurses and personal support workers were part of the health-care team. This is being piloted by a few Ontario Health Teams and should be further expanded and supported. Otherwise, patients are usually left to see a new nurse or personal support worker daily.
A mechanism must be put in place to ensure that primary care professionals who are not in an OHT or team-based care model have the same access to a care co-ordinator.
Benefits for physicians and the system
This model would lead to more effective and efficient communication between physicians, care co-ordinators and home-care providers.
The complexity of resident needs in long-term care is higher than ever. Long-term-care residents are often transferred to hospitals for diagnostic tests or treatments that could be done safely in the home if it was equipped with the necessary equipment and trained staff.
About half of long-term-care residents in Ontario who were transferred to an emergency department were discharged without being admitted to hospital, which means they spent their entire time in the ED, according to an earlier study. It also found that 24.6 per cent of residents were transferred for something that likely could have been treated in their home, most commonly pneumonia, urinary tract infections and congestive heart failure.
“Evidence has shown that we can prevent unnecessary transfers of long-term-care residents to hospitals by equipping homes with increased diagnostics. We can also help patients in hospital return sooner with IV administration in long-term care. Medical expertise and physician leadership are key to ensuring homes optimize the use of these resources” — Dr. Mohamed Abu-Abed, family physician and long-term-care medical director, Brampton, and chair, OMA section on Long-Term Care and Care of the Elderly
To prevent unnecessary hospital transfers of residents, all 630 long-term care homes in Ontario should have access to and/or be equipped with:
- Mobile diagnostic imaging clinics that provide on-demand (within 24 hours) access to in-home X-ray and ultrasound
- The ability to do same-day blood and urine tests to diagnose, treat or rule out a range of medical conditions
- The ability to administer IVs for fluids and medications
- A bladder scanner and an EKG machine
To ensure that all long-term care homes across the province have these tools, the government must allocate mobile diagnostic resources according to geography and population density.
Benefits for patients
Patients can avoid unnecessary hospital transfers.
Benefits for physicians and the system
This would make better use of health-care resources and reduce hospital overcrowding, as many of these patients end up occupying badly needed beds.
Too many people, who would prefer to die in the comfort of their own homes, are dying in hospitals. That is because there is insufficient palliative support available to meet patients’ needs. Moreover, there is inequitable access to services based on where a person lives. Individuals may qualify for palliative services in one part of the province, while Ontarians in other regions cannot access similar services.
The province should make meaningful progress toward 24/7 team-based care, including improving and expanding access to on-call/after-hours community specialists (including palliative specialists), especially for patients nearing the end of life. Hospice palliative patients cannot be managed during business hours. Patients need access to high-quality palliative care expertise, in all care settings, at all hours, every day, especially nearing the end of life.
Limitations in funding models create regional variations in how palliative care is delivered across the province. This creates inequities in funding allocation for palliative providers, further contributing to burnout in the community. The funding models were also not created with smaller communities in mind, making it difficult for continuous access to palliative expertise in these areas.
“It is vitally important that all Ontarians have access to equitable, universal, around-the-clock, high-quality palliative care. Patients suffer in our current postal code lottery. Where you live should not dictate the limits of the palliative-care services to which you are entitled. We must continue to fight for adequate funding to ensure that high-quality palliative-care systems and compassionate communities can exist everywhere. Governments need to understand that investing in palliative care enables choice in a patient’s place of care, saving health-care dollars and freeing up needed hospital beds. Palliative care is everyone’s responsibility” — Dr. Stephen Bernard Singh, family physician and palliative care specialist, Brantford
Primary providers in all care settings should also have increased access to regionally organized specialist palliative care resources, such as dedicated palliative consultation teams and specialized palliative programs and resources. These resources allow patients to stay close to home or in a home-like setting ensuring the expertise is available to support symptom management at end-of-life.
Benefits for patients
Patients will be able to die where they want to, rather than in a hospital, while receiving better care at end-of-life.
Benefits for physicians and the system
Ensuring all Ontarians have access to a palliative team, at the time of diagnosis of a life-limiting illness until death, will keep patients out of the emergency department and/or hospital if they do not require acute care.